This post is also available in:
Español (Spanish)
Français (French)
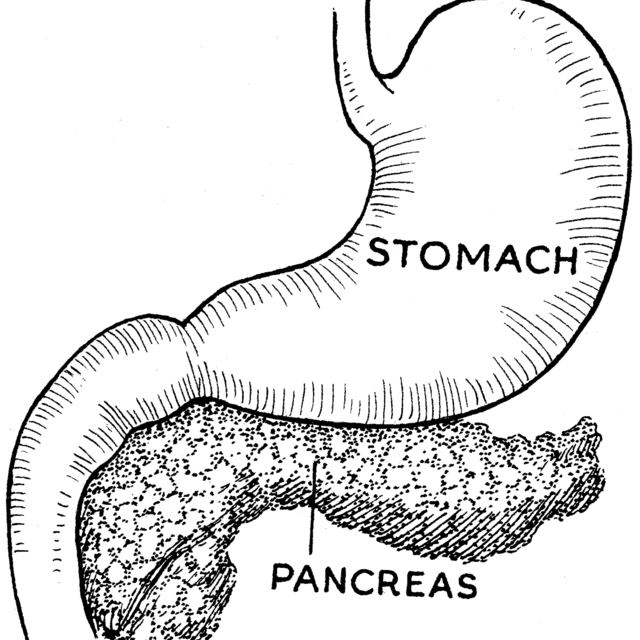
What is the pancreas?
The pancreas is an organ located in the upper abdomen, behind the stomach. The pancreas contains glands and ducts. The glands make important enzymes and hormones, which travel through the ducts and are released directly into the bloodstream or into the intestines.
What does the pancreas do?
The pancreas has two important jobs. First, it produces enzymes that help digest the food we eat. Problems with this function can lead to malnutrition and poor growth. The pancreas also makes important hormones like insulin, which helps manage blood sugar levels. Problems with this function can lead to diabetes.
What is acute pancreatitis?
Acute pancreatitis occurs when the pancreas becomes inflamed (swollen and irritated). This condition most often causes severe abdominal pain in the upper-middle and left sides of the abdomen. Nausea or vomiting may accompany the pain. Fever also can occur but is rare.
Acute pancreatitis is usually reversible, and most of the time it gets better on its own after several days or weeks. Severe complications are uncommon in children, and death is very rare.
What causes acute pancreatitis?
There are many causes of acute pancreatitis. Conditions such as gallstones, metabolic diseases such as high levels of fat in the blood, or infections can cause acute pancreatitis. Common medications that can cause pancreatitis include anti-seizure medications, certain antibiotics, and different types of chemotherapy. Sometimes injury to the abdomen from a playground accident or sports injury can cause acute pancreatitis.
In approximately 30% of cases of acute pancreatitis, the cause is unknown. These cases may be due to viral illnesses. Some patients may develop recurrent episodes of acute pancreatitis, or chronic pancreatitis. In these patients, additional investigations are needed to check for genetic or structural causes of the pancreatitis.
What are the signs and symptoms of acute pancreatitis?
The most common symptom is strong abdominal pain usually in the upper and left side of the abdomen. Often there is associated nausea and vomiting, although not all patients will have all of these symptoms. Some children may develop a fever or complain of back pain or even difficulty breathing.
If your child cannot verbalize pain, they may be more irritable, persistently cry, or will not let you touch their belly. It is important to remember that symptoms can be vague and can be similar to signs of other diseases such as viral gastroenteritis.
What tests are used to diagnose acute pancreatitis in children?
There is no single test for acute pancreatitis. When the pancreas is inflamed, it releases enzymes called amylase or lipase into the bloodstream. Doctors can measure these enzymes in the blood to diagnose pancreatitis. Sometimes a doctor will order an ultrasound of your child’s abdomen, which can show if the pancreas is swollen.
In more severe cases, a computed tomography (CT) scan can provide important information about the pancreas injury. However, CT scans are not done in mild cases to limit radiation exposure to the patient. Depending on the situation, magnetic resonance imaging (MRI) may be done instead of a CT scan.
Blood tests and radiology scans (ultrasound, CT, MRI) are not always abnormal. In this case, your doctor will determine if your child has pancreatitis based on your child’s history, severity, and symptoms.
What is the treatment for acute pancreatitis?
There is no specific medication to treat pancreatitis. Most doctors use supportive care until the condition resolves. Milder cases of pancreatitis may be treated at home, without hospitalization.
The best way to treat inflammation is to have your child drink plenty of fluids to maintain good hydration. Over-the-counter pain medications such as acetaminophen or ibuprofen can be used to help manage pain in mild pancreatitis.
If your child has persistent nausea or vomiting, your doctor may give anti-nausea medications. When the pain has improved and your child expresses a desire to eat, they can try to eat. The choice of food will depend on what your child can tolerate. If your child cannot eat and drink enough to maintain nutrition, they will need to be hospitalized.
Moderate to severe cases are admitted to the hospital for intravenous fluids and intravenous pain medications. Hospitalization usually lasts a few days. Once a child is no longer vomiting, liquid nutrition is recommended early if possible. Your child may be offered small amounts of liquid nutrition.
In cases of severe pancreatitis where a child cannot eat for many days, doctors may place a feeding tube through the nose and into the stomach or intestine to give liquid nutrition, or they may give intravenous nutrition. Nutrition is important in the healing process.
Rarely, the inflammation can be severe enough that other organs also become inflamed, and your child may need to be admitted to an intensive care unit for close monitoring.
In addition, your doctor may recommend other treatments for the underlying cause of the pancreatitis. For example, if gallstones caused your child’s pancreatitis, surgeons may remove the gallbladder once your child improves.
Can my child die from acute pancreatitis?
Death from acute pancreatitis is extremely rare in children, but it can happen. Most deaths associated with acute pancreatitis occur in children with significant illness that damages multiple organs or significant underlying medical problems.
What are the long-term complications if my child has acute pancreatitis?
Most cases of acute pancreatitis resolve, with no long-term complications. If the pancreatitis is severe, however, the most common complication is collection of fluid around the pancreas. This will develop over several weeks after the episode of pancreatitis.
These pancreatic fluid collections, sometimes called a “pseudocyst,” can go away over time. However, occasionally they can lead to ongoing abdominal discomfort, pain, or vomiting. If the pseudocysts persist or cause symptoms, your doctor can drain the fluid. Drainage may be performed by a special radiology procedure or a special endoscopy procedure, but it sometimes requires surgery. Rarely the fluid collections can become infected and require urgent drainage and treatment with antibiotics.
Does pancreatitis recur?
Approximately 15%–30% of children who have pancreatitis will have additional episodes. If your child has recurrent episodes, your doctor will carry out additional testing to determine the cause for the recurrent acute pancreatitis, including genetic tests.
Authors: Amit Grover, MD & Victor Fox, MD
Editor: Athos Bousvaros, MD
July 2021
This post is also available in:
Español (Spanish)
Français (French)