Accommodations
Overview
Although most children and young adults with inflammatory bowel disease (IBD) lead healthy and productive lives, it is common for individuals with IBD to have periods of severe illness that interfere with school, activities, and work. During these periods, a family member or caretaker may also need to take time off from work to care for the sick child.
These periods of severe illness or hospitalization are often stressful for children and parents. Your child may be thinking “How will I ever get back to school?” Parents or caretakers may be thinking “Will I lose my job?”, or “What if insurance won’t cover my child’s medications?”
Educational Accommodation Plans
Preschool, elementary, and secondary education:
- Section 504 refers to various educational settings. When possible, students with disabilities will be educated, have meals, and participate in activities with other students in the same facilities. If a child needs to use a facility other than the usual classroom, it must be as comparable to the usual classroom as possible.
- A Section 504 plan can include proximity to a bathroom, an anytime bathroom pass, stop the clock testing, tutoring, or other assistance when a child is unable to attend school due to illness. The aim of accommodations under Section 504 is to provide the child with a level playing field. Any accommodations under Section 504 must be provided for free.
- Federal regulations allow for your child to have a formal evaluation before they are provided with an educational accommodation plan. Such formal evaluations rarely occur under Section 504, although they are required under the Individuals with Disabilities Education Act (IDEA).
- If a child requires special education, then the plan will be an individual education plan (IEP) under IDEA. A Section 504 plan does not and cannot include special education services. However, 504 accommodations can be written into IEPs.
Postsecondary education:
- Section 504 and the Americans with Disabilities Act (ADA) require that undergraduate colleges prepare a plan to accommodate students’ disabilities.
- Regulations prohibit discrimination in admissions and recruitment. This means that colleges cannot exclude students with disabilities or set quotas (limits) for admission of students with disabilities.
- Students with disabilities cannot be excluded from any academic, research, occupational training, housing, health insurance, counseling, financial aid, physical education, athletics, recreation, transportation, or other extracurricular activities.
- Academic adjustments must be made to eliminate and/or protect against discrimination. Adjustments may include giving students more time to complete their degree requirements. Exams and evaluations may also be changed to ensure that the results of evaluation reflect the student’s performance and not their disability.
- Housing and financial assistance must be provided to students with disabilities to the same extent as they are provided to students without disabilities. Note that courts tend to defer more to colleges than to elementary and secondary schools regarding accommodations that schools claim affect academic integrity.
How does a child get a Section 504 plan?
If you want a Section 504 plan for your child, you must request a Section 504 meeting. The Section 504 team will include school officials, all or some of the student’s teachers, and parents.
How is a Section 504 plan created?
A Section 504 plan is created by the Section 504 team. You may bring a draft of a plan with you to the meeting, or the school may prepare the first draft. It is important to remember that Section 504 plans are a process of negotiation. There is nothing that must be included, and nothing, within reason, that cannot be included.
What if the Section 504 plan doesn’t work?
If you agree to a plan and it turns out to be insufficient, you can request another Section 504 meeting.
If you are unable to reach an agreement with the school about the Section 504 plan, you must follow any procedures the school district offers for dispute resolution (such as a hearing). If you are still dissatisfied with the school district’s response, you may file a complaint with the U.S. Department of Education Office of Civil Rights.
Problem areas for patients with IBD
Patients with IBD face two issues that are not well-addressed by the law.
First, children who do well in school are often expected to not need help. According to IDEA, the definition of a “child with a disability” is a child who, because of their disability, needs special education and related services. A student is not considered a “child with a disability” if they are performing well academically and do not need special education. Because many children with IBD do not suffer academically, they may not be covered under IDEA. However, children with IBD are still eligible for accommodation plans under Section 504.
Second, neither statute (Section 504 or IDEA) provides guidance for children with a chronic disease that remits and relapses (flares). The 2008 amendments to the ADA make a big difference here by stating that episodic illnesses are disabilities. As with any chronic illness, there will be times when a student needs home tutoring and other times when the student has no need for assistance. This presents a challenge for both the parents and the school because a Section 504 plan is not intended to apply only some of the time. Flexibility is difficult to build into a plan.
Disabilities can be temporary but still disabling. However, getting the school to respond quickly to constantly changing circumstances is a challenge. A plan under Section 504 may include accommodations such as seating placement, extended time for testing, adjustment of class schedules, use of aids such as digital recorders, class and/or homework assistance, administration of medications, behavioral support, and tutoring. Elements of such a plan are present, but the difficulty is coordination and timing.
How can your child’s health care team help?
School teachers and administrators are dedicated professionals whose goal is to educate children. In some instances, when a child is absent and/or not performing well in school, school professionals may suspect malingering (making up or exaggerating symptoms).
If you give permission, your child’s doctor or social worker can support your child by calling or writing to the school about your child. Once a school administrator hears from a health care professional, they will usually be more sympathetic to your child’s needs and issues.
- A sample letter of support for a 504 plan (school accommodations) can be found at Crohn's & Colitis Foundation.
- Bring this letter in to your child’s doctor and ask the provider to adapt it for your child.
- Your child’s doctor or social worker can also speak to school administrators and tell them about your child’s disability and medical history with IBD (including symptoms, medications, and hospitalizations). While such a call is not a substitute for a letter in support of a 504 plan, 5 minutes on the phone may save 5 hours of paperwork.
What about college?
Students with IBD who graduate from high school and go to college sometimes require assistance and are on their own for the first time. As mentioned above, Section 504 plans apply to public undergraduate colleges. Most public and private universities and colleges have a Disability Office where students can register. Making the school aware of the student’s illness and possible complications that could occur prior to school starting will help avoid possible problems during a time of a flare. A plan can be made with the Disability Office as to how a student should communicate with their professors and how schoolwork can be made-up in case an illness occurs.
More information about making a successful transition to college with IBD can be found at Crohn's & Colitis Foundation's Campus Connection.
Family and Medical Leave Act (FMLA)
What is the Family and Medical Leave Act?
Sometimes children with IBD may have a severe course with prolonged hospitalization, surgery, school absence, or intermittent absences for things like Remicade infusions. During these periods, parents and other caretakers may need to leave work to care for the sick child. When this happens, you may be emotionally and financially stressed. You may even be afraid of losing your job. FMLA was passed in 1993 to help with such difficult situations.
- FMLA was designed to help employees balance work and family responsibilities by allowing for reasonable unpaid leave for family or medical reasons. FMLA only applies to employers with 50 or more employees and only to employees who have been employed for 12 months (1,250 hours). Your state may have a law that applies to smaller employers. FMLA is enforced by the U.S. Department of Labor Employment Standards Administration, Wage and Hour Division. Employers must post a notice explaining the rights and responsibilities under FMLA and may be fined if they fail to do so.
- FMLA provides up to 12 weeks of unpaid leave in any 12-month period. The 12-month period can be calendar year, fiscal year, or a rolling 12-month period. During the 12 weeks of leave, the employee cannot be fired. The 12 weeks of leave may be taken intermittently. However, if leave is taken for treatments, reasonable effort must be made to not disrupt the employer’s operations. FMLA leave may be taken for many family and medical reasons, including:
- Birth and care of a newborn child
- Placement with the employee of a child for adoption/foster care
- Care of an immediate family member with a “serious health condition,” or the employee’s own “serious health condition”
A “serious health condition” is defined as:
- A condition that results in at least three consecutive full calendar days of incapacity needing inpatient care;
- A condition that requires continuing treatment by a health care provider and includes any period of incapacity lasting more than three consecutive days during which the individual needs treatment two or more times by a health care provider; or
- A serious chronic health condition that continues over an extended period of time, requires repeated visits to a health care provider, and may involve occasional episodes of incapacity.
- If the need for leave is foreseeable (known in advance), thirty days of notice is needed to take FMLA leave. Otherwise, the employer must be notified of the need for leave as soon as practical. Employees must also give enough information so the employer can decide if FMLA applies to the request (such as hospitalization, pregnancy, unable to perform functions of the job, family member under continuing care of a provider).
- The employer is required to make premium payments on health insurance to maintain the employee’s benefits while on leave. A 30-day grace period must be given before benefits may be cancelled. However, if the employee does not return to work for an appropriate reason, they may be required to reimburse the employer for those health insurance payments.
- Employees returning from FMLA leave must be reinstated to the same or equivalent job with the same pay, benefits, and terms and conditions of employment. Employees may take, or employers may require employees to take, any accrued paid vacation, personal, family, or medical/sick leave at the same time as FMLA leave (called substitution of paid leave).
- FMLA leave may be taken intermittently (a day here or there) and does not need to be used only for long-term absences.
How can your health care team help you with the family medical leave process?
To obtain FMLA leave, you must submit a written request to your employer. The health care provider must provide a medical certification of the need for absence. In most cases, all that is needed is a brief doctor’s note establishing that you or a family member has a serious health condition, as defined above. In some cases, you may need to ask a member of the health care team to fill out a form for the company or provide a more detailed letter of medical necessity. You are not required to provide medical records
Medication Coverage
What are patient assistance programs?
Patients with chronic illnesses such as IBD often have health-related expenses that add up over time. In addition, families of patients with IBD may go through periods without work or health insurance.
Patient assistance programs help patients and families who do not have insurance or do not have enough insurance. Some programs help patients access medications for little or no cost, based on financial eligibility. Other programs help reimburse some expenses that add up due to frequent co-pays or other costs, so that it is less likely a patient or doctor has to postpone a necessary test, procedure, or office visit.
Free medications
Almost all pharmaceutical (prescription drug) companies that manufacture medicines run a patient assistance program. To qualify for these, patients must show they have no insurance or have been denied coverage of a medication by their insurance company. Patients or families must also provide proof of income.
Patients or families can start the applications, but a portion of the application must be filled out and signed by the prescribing doctor. Applications often take 3–4 weeks for approval.
NeedyMeds
NeedyMeds has a lot of information and is easy to use. The website keeps an updated master list of every pharmaceutical company, brand name medication, or generic medication that has an affiliated patient assistance program. The website provides a direct link to each program’s website and contact information (if relevant).
RXHope
RXHope is a similar program that helps facilitate the process of finding and applying to patient assistance programs for certain medications. A health care professional or a family can set up a free account to register with the website and begin the process.
Partnership for Prescription Assistance
Partnership for Prescription Assistance's website has separate sections for patients, caregivers, or physicians. The website links to relevant patient assistance programs and can help you complete forms online.
RxAssist
RxAssist's website has a searchable database of patient assistance programs. You can search by drug name or pharmaceutical company. Once you find the company that makes the medication you need, you can write them and ask them for assistance with getting medication.
Co-pay assistance programs
There are separate programs available for patients or families who have insurance but have trouble paying for premiums/co-pays that add up when dealing with recurring costs. To qualify, patients or families must provide proof of income.
Patients or families must start the applications, but there is a section to be filled out by the doctor who is conducting visits, ordering lab work, etc. These programs usually work in a reimbursement format. If a family is approved, they must send in receipts for care provided.
Patient Access Network Foundation
Patient Access Network Foundation provides assistance for IBD patients. The program only covers the costs of medications or infusions. Benefits under this program are limited to $3800 per year, but eligible families can continue to re-apply each year. The program can run as a reimbursement for expenses already paid by the family or can pay expenses directly to a physician or hospital if coordinated by the family.
You can reach the Patient Access Network Foundation at 1-866-316-7263.
Other Assistance Programs
The Modest Needs Foundation provides one-time emergency grants to financially needy families or individuals.
For information on ostomy supply assistance, you may contact the following organizations:
The Osto Group (1-877-678-6690)
www.ostogroup.org
Friends of Ostomates Worldwide
www.fowusa.org
Email: info@fowusa.org
United Ostomy Associations of America (UOAA)
(1-800-826-0826)
www.ostomy.org
Convatec Access Program (1-800-422-8811)
meplus.convatec.com
Hollister (1-888-740-8999)
www.hollister.com
If you have further questions after reviewing the above information, you can contact the Crohn’s & Colitis Foundation at 1-800-932-2423 or info@crohnscolitisfoundation.org to get more information on medication and health insurance resources.
Insurance Options
What are insurance options for patients with IBD?
Health insurance is necessary for patients with IBD. There are two kinds of group insurance plans: self-funded plans and fully funded plans. Which kind of insurance plan you have might explain what your insurance is required to do under the law.
- Self-funded plans are plans under which the employer actually pays for the health care that is provided to the insured, and the insurer simply acts as a third-party administrator. Self-funded plans are governed solely by a federal law known as ERISA.
- Fully funded plans are what we all commonly think of as insurance. With these plans, the employer purchases coverage from an insurer who pays the claims. Fully funded plans are governed by state law.
Patients with IBD have several options for insurance:
- Insurance through a parent’s policy: If a patient is a minor and is in school, they may be eligible to be insured under their parent’s insurance. The patient will be covered up to 26 years of age or until they become eligible for health insurance through an employer, whichever is earlier.
- Group insurance through an employer.
- Individual insurance through public assistance (Medicaid, SCHIP).
What is COBRA?
Federal law mandates that patients be offered continuation of insurance at the patient’s expense after a job ends or after a child is no longer under a parents’ policy. This is called COBRA.
- If a patient decides to take COBRA after losing a job, they typically have up to 18 months of coverage. This can be
extended to 29 months if the patient has been found to be disabled by the Social Security Administration. If a patient decides to take COBRA after aging out of their parents’ policy, they will have 36 months of COBRA coverage. - The patient must pay the premium for the insurance plus a 2% administrative fee. Federal law requires employers to provide employees with COBRA information within 44 days of the qualifying event (end of the job or aging out of a parent’s insurance). Patients then have a designated period of time (typically 60 days) to sign up for COBRA (called election). If the COBRA election is made more than 30 days after the qualifying event, the patient will have to pay the COBRA premium for all of that time so that COBRA coverage goes back to the date of the qualifying event.
What is “HIPAA eligibility”?
A patient is HIPAA eligible if they:
- Have had 18 months of continuous insurance (the last day must have been in an employee-based plan).
- Have exhausted COBRA coverage; are not eligible for other insurance (i.e., group, Medicare, Medicaid).
- Do not have health insurance.
- Have not had a break in coverage of 63 days or more.
If you are HIPAA eligible, you must be offered a “guaranteed issue” policy. The “guaranteed issue” option differs from state to state. It may be the state’s “high risk pool,” which is a plan designed for people with pre-existing conditions. It may be each carrier’s most popular plan, or a choice of a high or low-deductible plan. In some states, it is a plan offered by Blue Cross. To find out what your state’s “guaranteed issue” plan is for HIPAA eligible individuals, call your state’s insurance department.
Insurance options for patients who are NOT HIPAA eligible:
- “High risk pool” for people with chronic illnesses: This is state-run and usually expensive.
- COBRA conversion policy (also called conversion policy): This policy allows patients to change their group policy into an individual policy when leaving the group policy or when their COBRA expires. These policies are expensive and usually do not have complete coverage.
- “Mandated issue/guaranteed issue” plans: Individual states require insurance companies to offer plans to those in need. These plans must be investigated on a state-by-state basis.
Letters of Medical Necessity
Letters of medical necessity are most often used to inform insurance companies of the need for a particular treatment.
They can also inform schools or others of the need for accommodation based on an individual’s health condition. Preparing such documentation is often time-consuming and requires the health care team’s input. Sample letters are available on the Crohn’s and Colitis Foundation’s Website in the professionals section.
These letters can be adapted by you or your medical team for your needs.
PLEASE NOTE THAT LETTERS OF MEDICAL NECESSITY MUST BE SIGNED BY A HEALTH CARE PROFESSIONAL, NOT BY THE PATIENT. The health care professional assumes responsibility for the precise content of the letter, which must be truthful and accurate. The sample letters are examples only, drafted to assist and educate your medical team.
Edited by Joann Niklinska-Schirtz March 2022
Created by NASPGHAN IBD Committee Advocacy Working Group
Chair: Mark Integlia MD
Working Group Members: Janis Arnold LICSW, Athos Bousvaros MD MPH, Cheryl Blank MD, Jennifer Jaff, Esq, Brad Pasternak MD
Tools
Web Resources

New Website IBD & Me Activity Center
The NASPGHAN Foundation along with the Crohn’s & Colitis Foundation of America (CCFA) a, has launched a new website called: IBD & Me Activity Center!
The IBD & Me Activity Center is a place for kids and parents to learn more about Crohn’s disease and ulcerative colitis, which are types of inflammatory bowel disease (IBD).
Here, you’ll meet some new friends and play some fun games, all while learning about IBD and how to manage it. Learning about your health is one of the best ways to take care of yourself.
Books
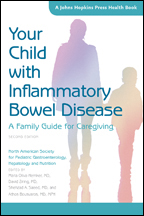
Your Child with Inflammatory Bowel Disease:A Family Guide for Caregiving – 2nd edition North American Society for Pediatric Gastroenterology, Hepatology and Nutrition edited by Maria Oliva-Hemker, MD, David Ziring, MD, Shehzad A. Saeed, MD, and Athos Bousvaros, MD, MPH
Inflammatory bowel disease (IBD) is a common condition in children and adolescents. Parents and other family members typically have many questions about the diagnosis, symptoms, and treatments associated with various forms of IBD including Crohn’s disease, ulcerative colitis, and indeterminate colitis. In this book, medical experts explain all you need to know about IBD and answer important questions, including:
- What are inflammatory bowel diseases, Crohn’s disease, and ulcerative colitis?
- Is there a cure for IBD?
- How is IBD going to affect my child’s daily life?
- Will my child’s diet change?
- Can my child still play sports?
- Will my child need surgery?
- What are the side effects of commonly prescribed medications?
- What challenges may my child face at school and socially, especially as he or she grows older?
This new edition has been thoroughly revised with updated scientific evidence. The chapters on medical therapies have been expanded to include robust discussions of emerging biologic medications and forms of nutrition used for treating IBD. A new chapter on complementary and alternative therapies expands on this topic. To purchase: Please go to the Johns Hopkins Press Website.