This post is also available in:
![]() Español (Spanish)
Español (Spanish) ![]() Français (French)
Français (French)
What is the Pancreas?
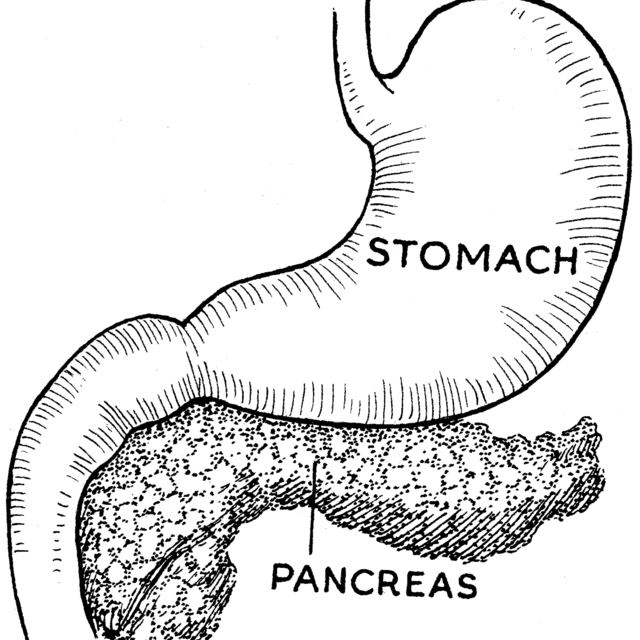
The pancreas is an organ located in the upper abdomen behind the stomach. The pancreas is an elongated organ in the middle and left upper abdomen. It is made up of glands and ducts. The glands make important enzymes and hormones, which are released directly into the bloodstream or into the intestines through the ducts.
What does the pancreas do?
The pancreas has two very important jobs. First, it produces enzymes that help digest the food we eat. Problems with this function can lead to malnutrition and poor growth. The pancreas also makes important hormones like insulin which help manage our blood sugar levels. Problems with this function can lead to diabetes.
What is Chronic Pancreatitis?
The term pancreatitis simply means inflammation of the pancreas. Pancreatitis may be either acute (a single episode), or chronic (many episodes, or ongoing inflammation. Chronic Pancreatitis occurs when there are changes, such as scarring, in the pancreas. It often results from repeated attacks of acute pancreatitis, which leads to damage and scarring to the organ. Over time, chronic pancreatitis eventually may result in decreased ability to produce digestive enzymes which impairs a child’s ability to digest food and make pancreatic hormones such as insulin.
What causes Chronic Pancreatitis?
Chronic pancreatitis is rare in children. There are many causes of chronic pancreatitis. The most common identifiable causes include genetic alterations, metabolic or anatomic abnormalities that result in multiple episodes of acute pancreatitis. However, the underlying cause may not be identifiable.
What are the signs and symptoms of Chronic Pancreatitis?
Frequent or chronic abdominal pain is the most common symptom of chronic pancreatitis. The pain can be constant, or can come and go unpredictably. Some patients however, have no pain at all. Children may also feel nauseous. Because the pancreas is scarred, it loses some of its function and ability to make enzymes that help digest food. If the pancreas is severely damaged, some children will have oily stools, diarrhea or weight loss. This is because they are unable to absorb what they eat. This may result in poor growth or poor weight gain, even though their appetite remains the same.
What tests are used in children to diagnose Chronic Pancreatitis?
There is no single test for chronic pancreatitis. The diagnosis requires the demonstration of irreversible damage to the pancreas, loss of digestive function or of diabetes (inability to make insulin). As symptoms can be vague and mimic other diseases, your gastroenterologist may carry out a combination of tests and studies in addition to asking about your child’s medical history and performing a thorough physical exam.
Most often blood and stool tests can show how a pancreas is functioning and whether or not it is producing enough enzymes for food digestion or insulin for sugar metabolism. Genetic tests can also be carried out to identify if a child has a gene mutation that increases their risk of chronic pancreatitis.
There are different radiological studies to look at the pancreas. An ultrasound can look for pancreatic swelling or inflammation. Computed tomography (CT scan) or magnetic resonance (MRI) can be used to look at the anatomy of the pancreas and assess the degree of damage. A special type of MRI called MRCP can show abnormalities in the pancreas better than an ultrasound examination. An endoscopic retrograde cholangiopancreatography (ERCP) (insert link to GI Kids ERCP) is a test that is performed by a qualified gastroenterologist that allows doctors to examine the ducts within the pancreas. ERCP can also be used to treat scarred areas of ducts, remove debris and help enzyme release by widening the duct opening (also called a sphincterotomy). This procedure requires anesthesia and specialized training/tools.
Blood tests and radiology scans, such as ultrasound, CT, or MRI, may not always be abnormal. In this case your doctor will make a judgement based on your child’s history, severity and symptoms.
What is the treatment for Chronic Pancreatitis?
There is no specific medication to treat pancreatitis; and currently there is no cure for chronic pancreatitis. Most doctors utilize supportive care to manage the complications of chronic pancreatitis. This may include giving medicine to help treat the pain or involving pain specialists who have expertise in chronic pain management. Pancreatic enzymes can be given to help children digest food when their pancreas is no longer able to make enough enzymes. In severe cases, insulin may be needed as well, to control the body’s sugar level.
If there is an anatomic abnormality, then an ERCP (see above) or surgery may help. Currently, there are no effective medical treatments for patients with a genetic mutation that leads to chronic pancreatitis.
For patients with chronic pancreatitis and chronic pain that does not improve, a surgical procedure can be considered. One surgical procedure is called a lateral pancreaticojejunostomy, also known as the Puestow operation. This procedure involves connecting a segment of small intestine to the pancreas to allow the pancreas to drain. Another procedure is called a Total Pancreatectomy and Islet Auto Transplant (TPIAT). In this procedure, the surgeon removes the pancreas and the hormone-producing cells known as ‘islets’ are isolated and returned to the patient by injecting them into the liver. TPIAT is a complex procedure and should be discussed with your gastroenterologist.
Is there a special diet for Chronic Pancreatitis?
There is no clear evidence to suggest that a special diet is required for chronic pancreatitis in children. Patients that have lost the ability to digest food, because of reduced pancreatic function, will be prescribed pills containing pancreatic enzymes to help with digestion. They may also be prescribed vitamins (A, D, E and K) since these levels may drop in patients with chronic pancreatitis.
Can my child die from chronic pancreatitis?
While chronic pancreatitis is a serious condition, death from chronic pancreatitis is rare in children.
What are the long term complications if my child has chronic pancreatitis?
The most common long term complication in patient with chronic pancreatitis is chronic pain. Some children may lose function of their pancreas and need medications, such as enzymes or insulin, to help them grow and live healthy lives.
Some children may develop fluid collections, or cysts, in or around the pancreas. They may also develop stones in the ducts, similar to kidney stones, which may cause pain attacks.
Adults with chronic pancreatitis have an increased risk of developing pancreatic cancer compared to the general population. The degree of risk depends on the underlying cause of pancreatitis and should be discussed with your gastroenterologist.
Authors: Amit Grover, MD & Victor Fox, MD
Editor: Athos Bousvaros, MD
July 2021
This post is also available in:
![]() Español (Spanish)
Español (Spanish) ![]() Français (French)
Français (French)